How Thyme Care Interventions Reduce Total Cost of Care
In 1995 when I decided to apply for oncology fellowship, one of the core drivers of my decision was my expectation, or at least my belief, that the field of cancer medicine would continually evolve and get better. And certainly in my 20+ years of practicing, that has been true. While there is still much work to be done, the advancement in treatment options for our patients has been staggering. But I also saw a future in which the existing fragmentation in care, the struggle that cancer patients had to go through to navigate the complex care landscape, would also get dramatically better.
Unfortunately it hasn’t. Far too many people with cancer suffer not only because of what cancer does to their body, but because they can’t navigate the system. As a result, too many people fall through the cracks, resulting in a poor patient experience, sub-par outcomes, and unnecessary care utilization.
As I’ve written and spoken about many times, it is well-established that care navigation (programs that provide patients with guidance and support along their care journey) can have a measurable impact on improving outcomes and costs in cancer care. Countless studies have shown that navigation can enhance the patient experience, keep people out of the hospital, lower costs, and even improve survival. However, these studies have been largely focused within single institutions or a single network of practices, begging the question: what impact would we see if cancer navigation were widely available to more patients?
At Thyme Care, we know the benefits that cancer navigation can provide, and want even more patients to have access. So we built a platform that takes the learnings that already exist, and enables them to scale. Our navigation solution pairs nurses and lay health workers with technology and data to enable appropriate, timely interventions that extend the reach and capacity of care teams to impact a broader set of patients.
As we took responsibility for navigating our health plan partner’s cancer members in New Jersey, we knew we were heading in the right direction. Feedback from patients was positive. The clinicians taking care of those patients appreciated our collaborative approach, liked working with us and welcomed our help. Our technology and operations helped standardize and control quality in ways that allowed us to scale. But we knew that one of the barriers to achieving our goal of making navigation widely available was to demonstrate our ability to improve quality while reducing costs.
So we set out to conduct a robust, propensity score-matched analysis to assess whether across a broad geographic population, with multiple practice types, Thyme Care could drive quality and reduce the total cost of care. Through our analysis, we showed that we were able to keep people with cancer out of the hospital and have a measurable impact on total cost of care, similar to what previous studies within a single institution or a single network of practices had shown.
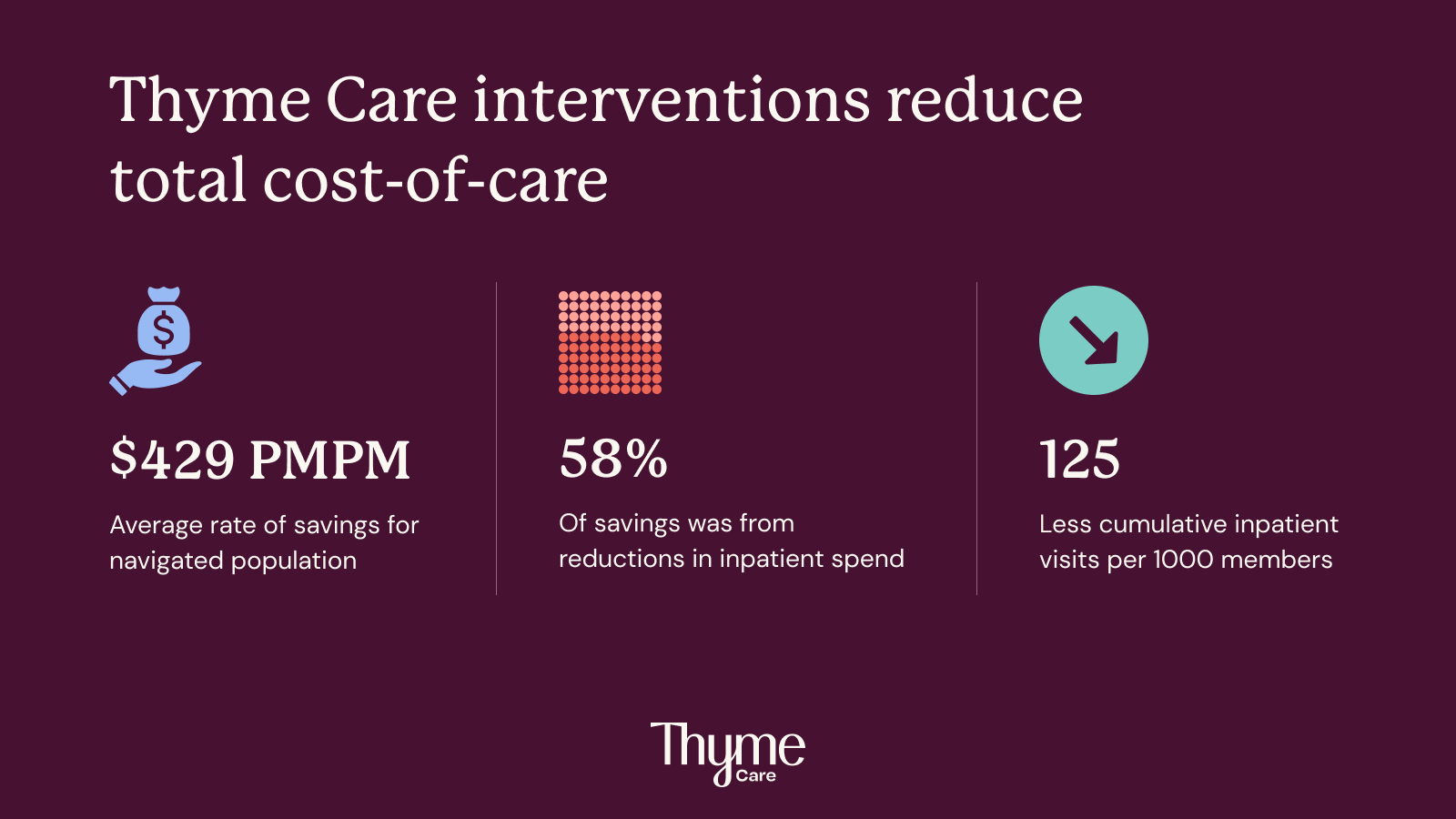
Thyme Care interventions reduce total cost of care by $429 PMPM.
We were not the first to try to analyze the impact of navigation interventions, and so to conduct our analysis, we recreated the methodology used by a frequently cited study in JAMA oncology from 2017. Using claims data for a NJ-based Medicare Advantage population, our analysis compared total medical costs (excluding part D drugs) of actively treated cancer patients navigated by Thyme Care to a matched control group from the same population.
The results of the analysis were extremely encouraging. For members that were navigated by Thyme Care, total cost of care decreased -$429 more per member per month compared to the control group. Just as notably, 58% of that reduction was attributable to inpatient spend. Given Thyme Care’s acuity-based engagement model specifically targets acute care utilization, these results were significant and served to validate the impact of our model.
The analysis showed a measurable impact on outcomes as well. At ten months post enrollment, our model indicated that the average cumulative inpatient admission rates were 7% lower for the navigated group compared to the control group.
We’re excited to share that our analysis was accepted by the American Society of Clinical Oncology (ASCO) for an oral abstract presentation, taking place at the ASCO Quality Care Symposium later this week.
What’s next?
Through this analysis, we’ve shown that independent, technology-enabled, cancer navigation can have a notable impact on cost and outcomes. But our work is far from over. We’re continuing to expand our partnerships with more health plans and providers, furthering our reach and ability to provide cancer navigation to even more patients who need it. This study is one very important step in a long journey towards our mission of making the cancer experience better and more affordable for everyone.
Learn more about how Thyme Care is improving outcomes and lowering costs: https://www.thymecare.com/health-plans.